Anyone can help prevent suicide — you don’t have to be a mental health professional. There are countless examples of silent heroes who recognize emotional suffering in people, respond compassionately to someone in distress, and then take action to promote healing and offer hope.
Listen to just one inspiring example. When an empathetic stranger confronted someone planning to jump off of a bridge, the young man found the courage and determination to give life
another chance.
Many of us worry we wouldn’t know what to do in that circumstance. To help promote more silent heroes, the National Suicide Prevention Lifeline created the
#Bethe1To campaign. If you believe someone may be at risk of suicide, or you recognize
warning signs of suicide, follow these clinically proven steps to #Bethe1To communicate with someone who may
be suicidal.
Step 1: Ask. There is a myth that asking about suicide increases suicidal thoughts. On the contrary, asking about suicide in a direct, non-judgmental way reduces
suicide ideation and gives people an opportunity to talk about their emotional suffering. As Dr. Barbara Moser, chair of Prevent Suicide Greater Milwaukee, describes in
this podcast, asking people in a direct way if they are thinking about killing themselves often brings relief. She shares three tips for how to initiate the conversation.
· First, preface the question. Before asking about suicidal thoughts or intent, mention your care and concern and what you have observed or heard that makes you think someone is suicidal. For instance, “I know you have a lot going on right now and have been feeling pretty hopeless and miserable. I’m concerned about you. Are you thinking about suicide; are you thinking about killing yourself?”
· Second be specific. Rather than ask “Are you thinking of hurting yourself?” ask instead, “Are you thinking about suicide?” or “Are you thinking about killing yourself?” Though this can be a difficult question to ask, it gets to the heart of your concern, makes responses easier to interpret, and communicates that you are open to talking about suicide.
· Third, take responses seriously. If responses are ambiguous, don’t let it go; circle back and ask again. If someone does share feelings of being suicidal, find out more about what is going on – both more about their emotional suffering (What’s going on?), as well as their reasons for living (What brings you joy? And what has kept you alive until today?”).
Step 2: Keep them safe. The second step first involves an assessment about a person’s safety and plans. As Dr. Moser describes, this is a time for blunt, direct questions that help you determine if a person has a plan and the means and intent to enact their plan. Questions to consider, include: “Do you think that you would act on those thoughts?” and “Have you thought about what you might do? Do you have a plan?” If they have a plan, you will also want to determine if they have access to their intended method. Keeping them safe then becomes about developing a safety strategy to decrease access to their chosen means.
Step 3: Be There. Just being there helps establish connection and feelings of belongingness, both of which are key protective factors that decrease suicidal ideation and action. Stay with the person, or if you are unable to, think of who else might be available to help. The suicide crisis is often acute, so being present with someone may help them ride out the time in which they are in the most immediate danger. To hear a story exemplifying the power of connection, listen to the story of
Travis Pipes, who reached out to a stranger “at a desperate time when he wasn’t having connected conversations with others.” There is power in patient, non-judgmental listening. There is hope in connection.
Step 4: Connect with Resources and Supports. Build a circle of support. This may mean helping the person connect with local resources, treatment professionals, and/or crisis counselors. It may mean helping initiate conversations with loved ones. It is recommended that you add the suicide prevention hotline (1-800-273-8255) and/or text line (Text “HOPELINE” to 74174) to your phone to increase access to crisis supports, which provide 24/7 free and confidential support. Finally, if someone is acutely suicidal, this may mean calling 911 so police can have the person evaluated by a professional. Getting immediate, appropriate help trumps confidentiality.
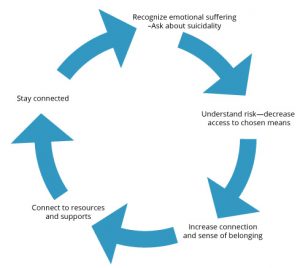
Step 5: Follow up. Reach out. Show continued support whether in person, via phone, text, or a card. Small gestures to check in can increase the feeling of connectedness. Simply letting people know you are thinking of them can make a big difference.
Connection and compassionate action are fundamental to all of these steps that can provide hope and support to people experiencing emotional pain and crisis. To learn more about how you can recognize warning signs of suicide, help someone in a crisis, and become a silent hero, consider attending QPR (Question, Persuade, Refer) gatekeeper training, either
locally or
online.
Thank you,
Sarah and the Wise Team
For support and resources, please call the National Suicide Prevention Lifeline at 1-800-273-8255 or text 741-741 for the Crisis Text Line. The podcast highlighted in this blog was produced by Giving Voice to Depression.  Step 5: Follow up. Reach out. Show continued support whether in person, via phone, text, or a card. Small gestures to check in can increase the feeling of connectedness. Simply letting people know you are thinking of them can make a big difference.
Connection and compassionate action are fundamental to all of these steps that can provide hope and support to people experiencing emotional pain and crisis. To learn more about how you can recognize warning signs of suicide, help someone in a crisis, and become a silent hero, consider attending QPR (Question, Persuade, Refer) gatekeeper training, either locally or online.
Thank you,
Sarah and the Wise Team
For support and resources, please call the National Suicide Prevention Lifeline at 1-800-273-8255 or text 741-741 for the Crisis Text Line. The podcast highlighted in this blog was produced by Giving Voice to Depression.
Step 5: Follow up. Reach out. Show continued support whether in person, via phone, text, or a card. Small gestures to check in can increase the feeling of connectedness. Simply letting people know you are thinking of them can make a big difference.
Connection and compassionate action are fundamental to all of these steps that can provide hope and support to people experiencing emotional pain and crisis. To learn more about how you can recognize warning signs of suicide, help someone in a crisis, and become a silent hero, consider attending QPR (Question, Persuade, Refer) gatekeeper training, either locally or online.
Thank you,
Sarah and the Wise Team
For support and resources, please call the National Suicide Prevention Lifeline at 1-800-273-8255 or text 741-741 for the Crisis Text Line. The podcast highlighted in this blog was produced by Giving Voice to Depression.